Ovarian Cancer Overview, Early Detection, and Screening
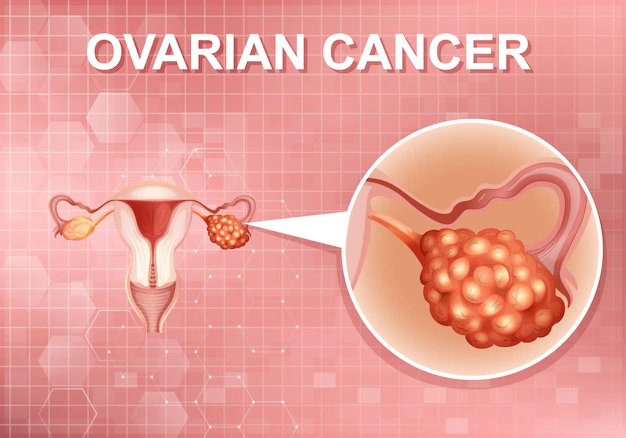
Ovarian cancer accounts for about 3% of all cancers diagnosed in women. But it is the fifth leading cancer killer of women.
- It’s most commonly diagnosed in women over age 50.
- About 1 in 78 women will develop ovarian cancer during her lifetime.
Researchers have found a handful of risk factors associated with ovarian cancer. The most important is a family history of breast or ovarian cancer. Other risk factors include:
- An inherited mutation of the BRCA1 and BRCA2 genes (the same genetic factor linked to breast cancer risk)
- The use of estrogen without progestin after menopause
- Smoking
- Never having had children or having a first child after age 30
- Excess weight also may play a role
- Incidence also rises with age, as half of all ovarian cancers occur in women over age 63
But most women who develop the disease don’t have any known risk factors.
The disease is hard to detect. And it is usually diagnosed at an advanced stage. This is why it is rarely curable. Only about 46% of women are alive five years after a diagnosis of ovarian cancer. However, occasionally the cancer is found at an early stage. This happens in about 15% of cases. The five-year survival rate is around 94%.
Finding ovarian cancer sooner rather than later
Early detection of ovarian cancer is hard. No standard screening test exists for the disease. And symptoms in the early stages tend to be unclear and can be linked to other health problems. But studies have identified some symptoms that are more likely to occur in women with ovarian cancer than in the general population. The most common are:
- Bloating
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Feeling a frequent or urgent need to urinate
It is recommended that if a woman develops any of these symptoms daily or almost daily and the symptoms persist for more than two or three weeks, she should see a doctor right away.
Of course, these symptoms can be caused by any number of ailments. And in most cases the problem won’t turn out to be ovarian cancer. If cancer is a possibility, various tests, including transvaginal ultrasound, may be recommended. This is performed with a thin instrument placed in the vagina.
Screening for ovarian cancer
Many women have undergone routine screening for ovarian cancer. This is often with a blood test called CA-125. This test measures a protein marker in the blood that can be elevated in women with ovarian cancer.
But an FDA warning issued in September 2018 said that women should not be regularly tested for ovarian cancer. They said that none of the tests are sensitive enough to reliably screen for ovarian cancer without a high number of inaccurate results.
The tests are widely used. But there’s no evidence that they reduce ovarian cancer deaths in women at average risk for the disease. The screening tests (transvaginal ultrasound and CA-125 blood test) often result in false-positives. This can lead to unnecessary surgery and complications.
- Women should be aware that there is currently no safe and effective ovarian cancer screening test.
- Women should not rely on ovarian cancer screening test results to make health or treatment decisions.
- Instead, talk to your doctor about ways to reduce the risk of developing ovarian cancer. This is especially true if you have:
- Family history of ovarian cancer
- BRCA1 or BRCA2 genetic mutations
- The updated recommendation does not apply to women at elevated risk for ovarian (or breast) cancer due to family history. These women should discuss genetic testing and screening with their doctor.
- And women with new or unusual symptoms that persist for more than two weeks should see their doctor. These may be early signs of the disease.
- This includes bloating, abdominal pain or pressure, urgent or frequent urination, or difficulty eating or feeling full quickly.
