Seven Things You Should Know About Vasectomy
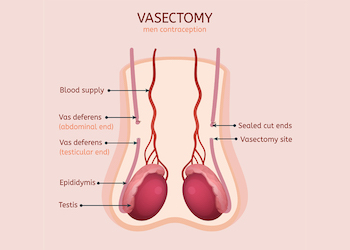
A vasectomy is a surgical procedure that involves cutting or blocking the vas deferens, the tubes that carry sperm from the testicles to the penis. Here are seven things you should know about vasectomy:
- It’s a highly effective form of birth control: Vasectomy is one of the most effective forms of birth control, with a success rate of over 99%. It’s considered a permanent method of contraception, although it may be possible to reverse the procedure in some cases.
- It’s a relatively simple procedure: Vasectomy is a relatively simple procedure that can be done in a doctor’s office or clinic. It typically takes about 30 minutes and can be done under local anesthesia.
- It doesn’t affect sexual function: Vasectomy does not affect a man’s ability to have an erection or enjoy sex. It only prevents the release of sperm during ejaculation.
- It takes time to become effective: It takes time for a vasectomy to become effective, and men should continue to use other forms of birth control until a semen analysis confirms that there are no sperm in their semen. This can take several weeks to several months.
- It’s a low-risk procedure: Vasectomy is a low-risk procedure, with few complications. However, as with any surgery, there is a small risk of bleeding, infection, and other complications.
- It’s a personal decision: Deciding to get a vasectomy is a personal decision that should be made after careful consideration of all the options. It’s important to talk to a healthcare provider and discuss the potential risks and benefits of the procedure.
- It’s reversible in some cases: Although vasectomy is considered a permanent method of contraception, it may be possible to reverse the procedure in some cases. However, the success of a vasectomy reversal depends on a number of factors, including the length of time since the vasectomy and the type of procedure that was done.
In summary, vasectomy is a highly effective form of birth control that is relatively simple and low-risk. It doesn’t affect sexual function and is considered a permanent method of contraception, although it may be possible to reverse the procedure in some cases. It’s a personal decision that should be made after careful consideration of all the options, and it’s important to talk to a healthcare provider and discuss the potential risks and benefits of the procedure.
